Fertility Preservation: Exploring the Options – Artificial Insemination vs IVF
Fertility is a complex and delicate aspect of human life, and for many individuals and couples, the ability to conceive a child is a deeply desired goal. However, for some, fertility may be compromised due to various factors such as age, health conditions, or medical treatments. In such cases, fertility preservation techniques become crucial in order to have the possibility of starting a family in the future. Two of the most common options for fertility preservation are artificial insemination and in vitro fertilization (IVF). In this blog post, we will explore the differences between these two methods, their success rates, and the factors to consider when choosing the best option for fertility preservation.
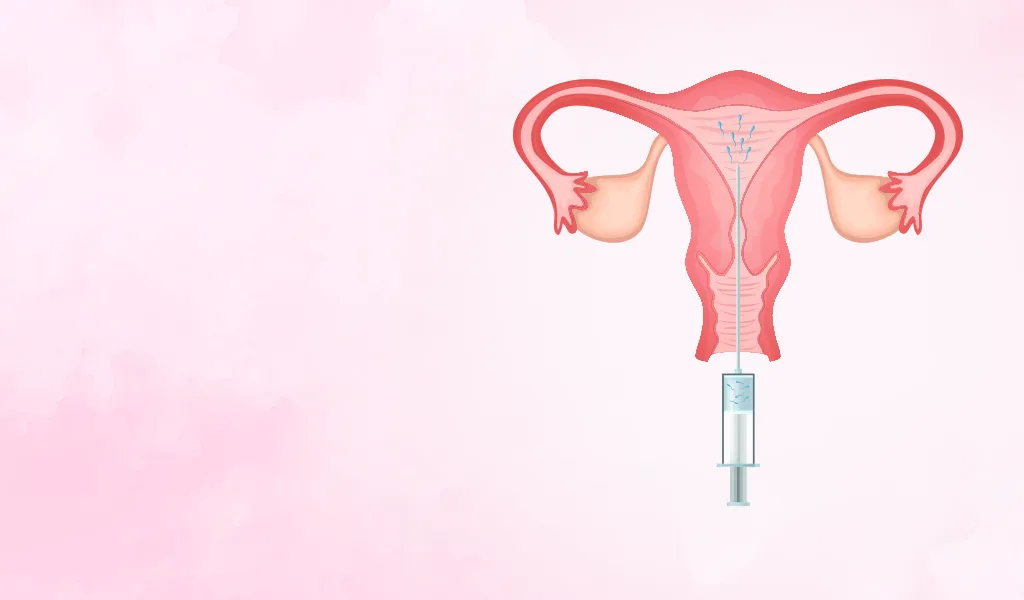
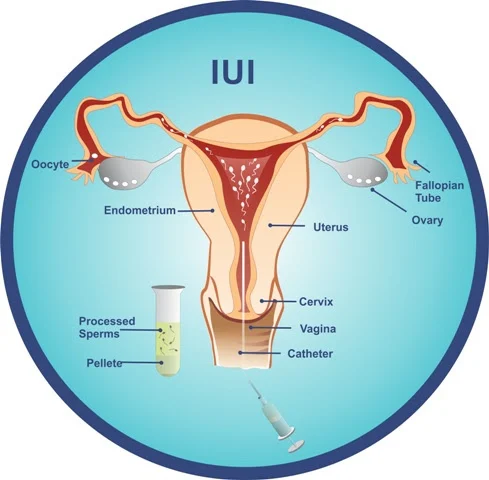
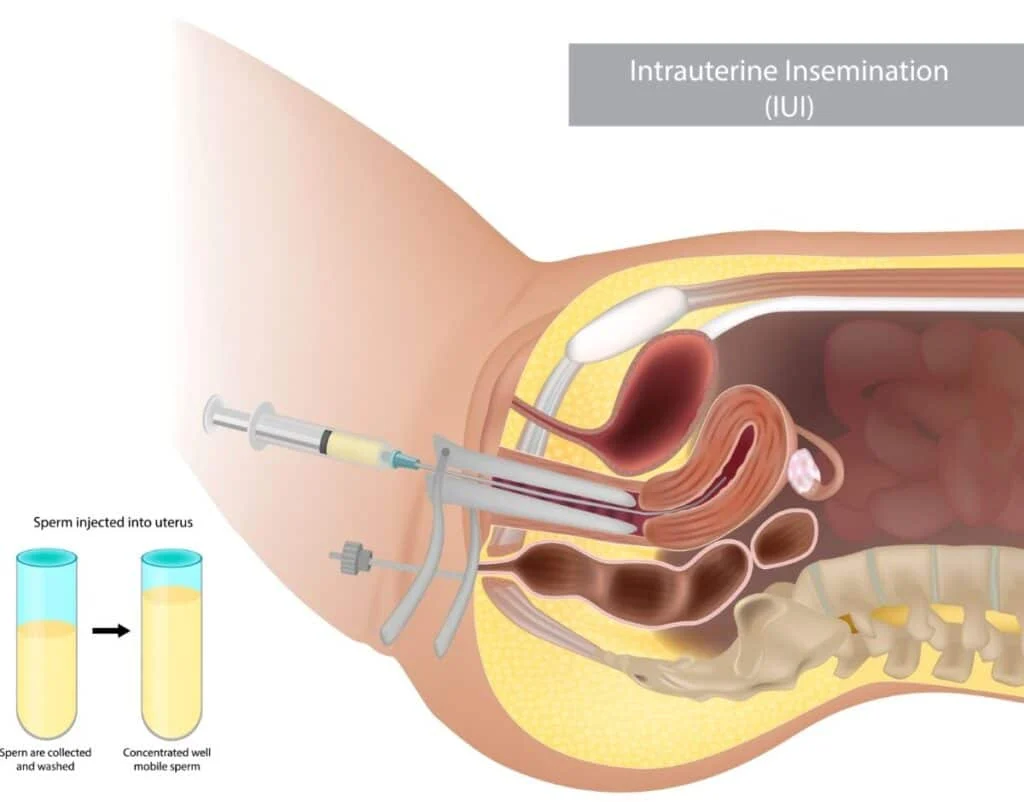
Artificial Insemination:
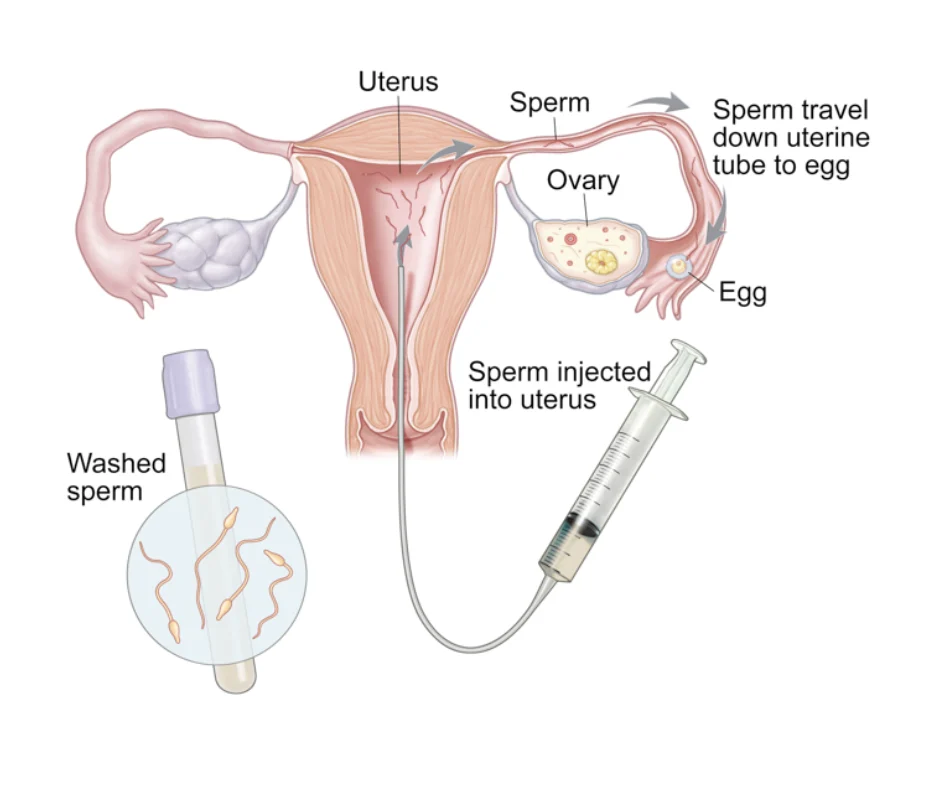
Artificial insemination, also known as intrauterine insemination (IUI), is a fertility treatment that involves placing sperm directly into a woman’s uterus, bypassing the cervix. The sperm used for this procedure can come from a partner or a sperm donor. This method is often used for couples struggling with male factor infertility or for single women and same-sex couples who want to conceive using donor sperm.
The process of artificial insemination starts with the stimulation of the ovaries to produce multiple eggs. Once the eggs are mature, a semen sample is collected and washed to remove any impurities. The washed sperm is then placed directly into the uterus using a thin catheter. This method is relatively simple and does not require any anesthesia, making it less invasive and more affordable compared to other fertility treatments.
Success rates of artificial insemination vary depending on factors such as age, sperm quality, and the cause of infertility. On average, the success rate for each cycle of artificial insemination is around 10-20%, and multiple cycles may be needed to achieve a pregnancy. This method also carries a slightly higher risk of multiple pregnancies compared to IVF.
In Vitro Fertilization (IVF):
In vitro fertilization (IVF) is a more complex fertility treatment that involves retrieving eggs from the ovaries and fertilizing them with sperm in a laboratory. The fertilized eggs, or embryos, are then transferred back into the uterus, where they can hopefully implant and result in a pregnancy. IVF is often recommended for individuals or couples with more severe fertility issues, such as blocked fallopian tubes, endometriosis, or low ovarian reserve.

Fertility Preservation: Exploring the Options – Artificial Insemination vs IVF
The process of IVF begins with the stimulation of the ovaries to produce multiple eggs. The eggs are then retrieved through a minor surgical procedure and combined with sperm in a laboratory. Once fertilization occurs, the resulting embryos are monitored for several days before being transferred into the uterus. The entire process may take several weeks to complete and may require anesthesia for the egg retrieval procedure.
The success rates of IVF also vary depending on factors such as age, embryo quality, and the cause of infertility. On average, the success rate for each cycle of IVF is around 30-40%, and the chances of success increase with multiple cycles. IVF also carries a higher risk of multiple pregnancies, which can be reduced by transferring a single embryo instead of multiple.
Factors to Consider:
When deciding between artificial insemination and IVF for fertility preservation, there are several factors to consider. Firstly, the cause of infertility plays a significant role in determining the most suitable method. For individuals or couples with mild fertility issues, artificial insemination may be a good option. However, for those with more severe fertility problems, IVF may be the better choice.
Age is also an important factor to consider, as fertility decreases with age, and the chances of success with any fertility treatment diminish as well. For women over the age of 35, IVF may be recommended as it offers higher success rates compared to artificial insemination. Additionally, the cost and invasiveness of each method should also be taken into account, as they can vary significantly.
Lastly, it is essential to discuss the potential risks and side effects of both methods with a fertility specialist before making a decision. Both artificial insemination and IVF carry risks such as infection, bleeding, and ovarian hyperstimulation syndrome. It is crucial to weigh these risks against the potential benefits and make an informed decision.
In conclusion, fertility preservation is a valuable option for those who wish to have children in the future. Artificial insemination and IVF are two of the most commonly used methods for fertility preservation, each with its own advantages and success rates. When considering these options, it is crucial to consult with a fertility specialist and consider factors such as the cause of infertility, age, cost, and risks. With the advancements in reproductive technology, individuals and couples now have the opportunity to preserve their fertility and fulfill their dreams of starting a family.