Intrauterine Insemination (IUI) and In Vitro Fertilization (IVF) are two commonly used fertility treatments for couples struggling to conceive. These assisted reproductive technologies (ART) offer hope to those facing infertility, but they differ in their procedures and success rates. As someone who has personally gone through both IUI and IVF, I want to share my story and compare these two treatments.
My husband and I had been trying to conceive for over a year without success. After various tests and consultations, we were diagnosed with unexplained infertility. Our doctor recommended starting with IUI, a less invasive and less expensive option compared to IVF. I was hopeful and excited, but also nervous about what the process would entail.
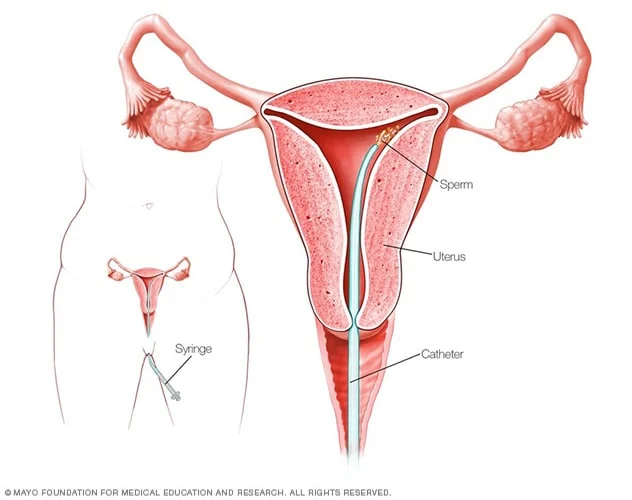
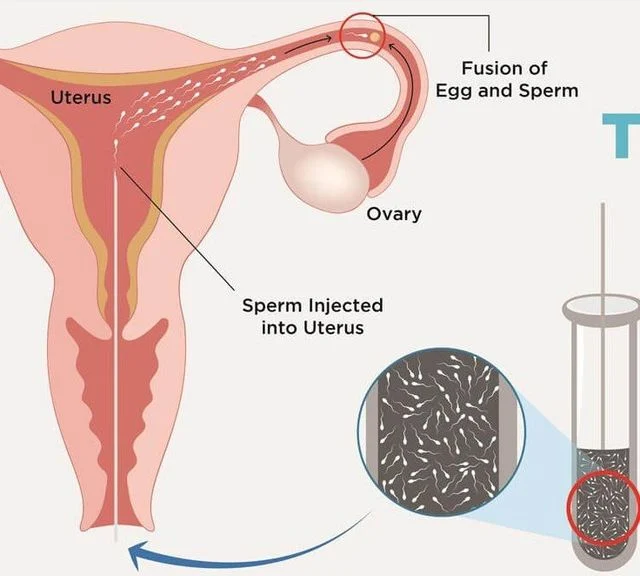
IUI involves placing washed and concentrated sperm directly into the uterus during ovulation. This procedure can be done with or without fertility drugs. In our case, we opted for the use of fertility drugs to increase the chances of ovulation and pregnancy. The process was simple and painless, and we were able to do it at our doctor’s office. However, it did require frequent visits for ultrasounds and monitoring to determine the best time for the procedure.
Unfortunately, our first IUI cycle was unsuccessful. We were disappointed, but our doctor reassured us that it often takes multiple cycles to achieve pregnancy. So, we tried again the following month, and this time, we were successful! I was overjoyed when we saw those two pink lines on the pregnancy test. However, our happiness was short-lived as I experienced a miscarriage at six weeks. It was devastating, but we didn’t lose hope and decided to try IUI again.
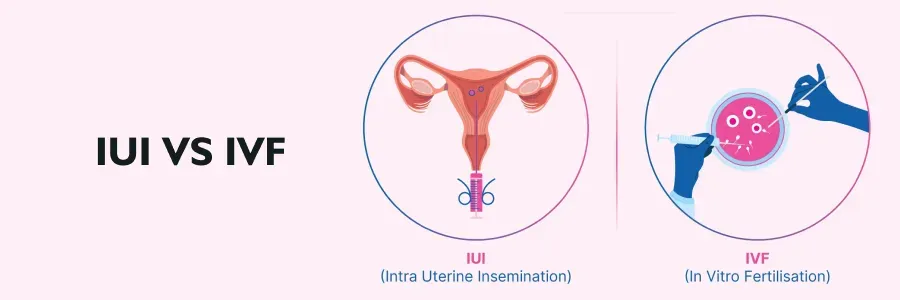
After three failed IUI cycles, our doctor suggested moving on to IVF. IVF involves retrieving eggs from the ovaries and fertilizing them with sperm in a laboratory. The resulting embryos are then transferred back into the uterus. This process is more invasive and expensive compared to IUI, but it also has a higher success rate.
Intrauterine Insemination vs In Vitro Fertilization: A Personal Story
The thought of IVF was daunting, but we knew it was our best chance of conceiving. The process began with daily hormone injections to stimulate my ovaries and produce multiple eggs. This was followed by egg retrieval under sedation, which was a bit uncomfortable but not overly painful. The retrieved eggs were then fertilized with my husband’s sperm in the lab, and we waited for five days for the embryos to develop.
The embryo transfer was the most nerve-wracking part of the IVF process. We had four embryos, and our doctor recommended transferring two to increase our chances of success. The procedure was quick and painless, and we were able to see the embryos on the ultrasound screen. The two-week wait to find out if the transfer was successful was the longest two weeks of my life. But when we got the call that I was pregnant, we were overjoyed and grateful.
Our IVF journey was not without its challenges. I had to administer daily hormone injections and go through numerous appointments and procedures. The emotional toll was also significant, with the constant rollercoaster of hope and disappointment. But it was all worth it when we welcomed our beautiful twin girls into the world.
Looking back, I can see the differences between IUI and IVF and how they impacted our journey. IUI was a less invasive and less expensive option, but it also had a lower success rate. IVF, on the other hand, was more physically and emotionally demanding, but it gave us our miracle babies. I believe that both treatments have their place in the world of fertility treatments, and the choice should be based on individual circumstances and preferences.
In summary, Intrauterine Insemination (IUI) and In Vitro Fertilization (IVF) are two popular fertility treatments that offer hope to couples facing infertility. IUI is a less invasive and less expensive option, while IVF is more invasive and expensive but has a higher success rate. As someone who has gone through both treatments, I believe that each has its own benefits and drawbacks, and the decision should be made based on individual factors.