Bringing Home a Baby: The Outcome of Artificial Insemination and IVF
Bringing a baby into the world is one of the most exciting and rewarding experiences in life. However, for some couples, conceiving a child is not as simple as it may seem. In recent years, advancements in medical technology have made it possible for couples struggling with infertility to still have a child of their own, through the use of artificial insemination and in-vitro fertilization (IVF). These methods have become increasingly popular, but there are still many questions and misconceptions surrounding them. In this blog post, we will explore the outcomes of artificial insemination and IVF and the impact they have on families who have chosen to use them to bring a child into their lives.
What is Artificial Insemination?
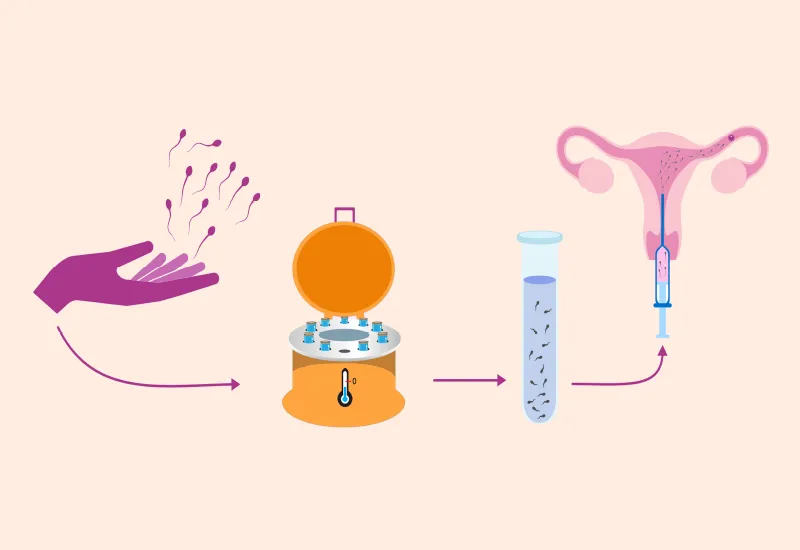
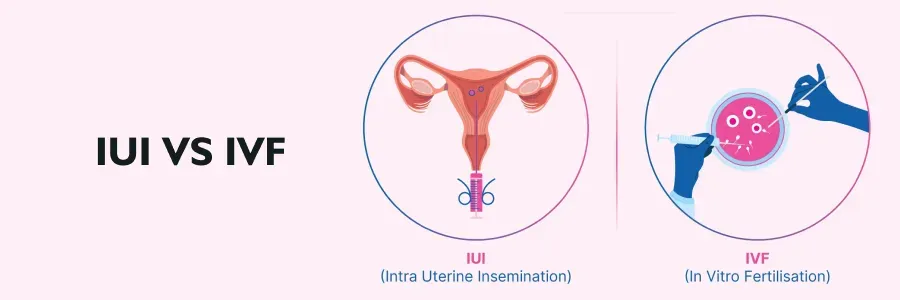
Artificial insemination is a fertility treatment that involves placing sperm directly into a woman’s uterus or cervix to increase the chances of fertilization. This procedure is often used for couples who have been trying to conceive for a while with no success, as well as for single women and same-sex couples. There are two types of artificial insemination: intrauterine insemination (IUI) and intracervical insemination (ICI).
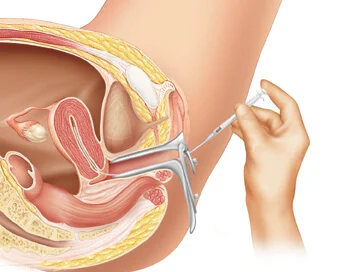
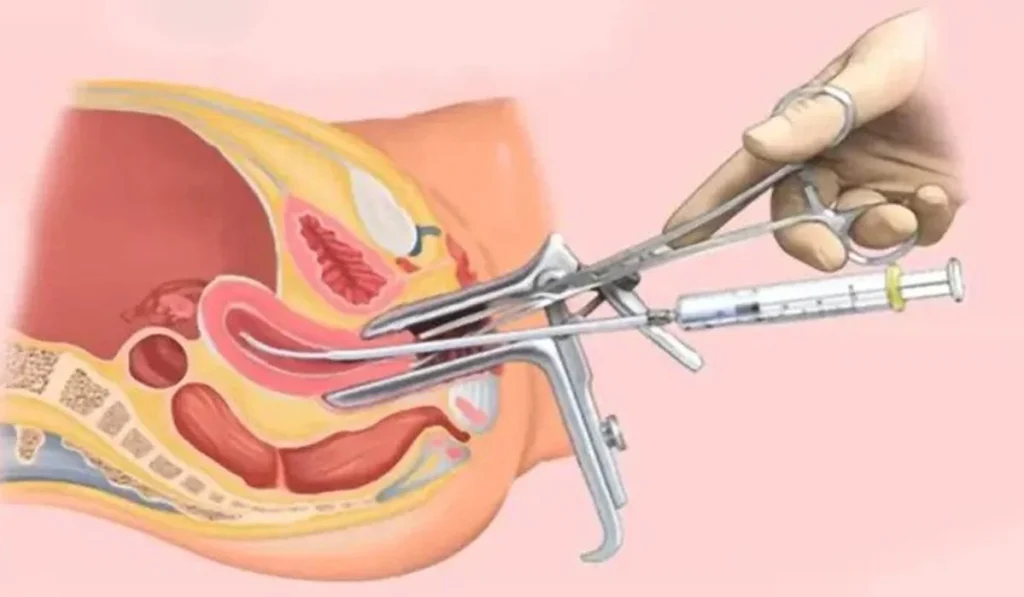
During IUI, a doctor will insert washed and concentrated sperm directly into the uterus through a thin tube. This is typically done around the time of ovulation when the chances of conception are highest. IUI can be performed with a partner’s sperm or donor sperm, depending on the couple’s situation.
With ICI, the sperm is placed in the cervix rather than the uterus. This method is less commonly used but is an option for those who cannot undergo IUI for medical reasons.
What is IVF?
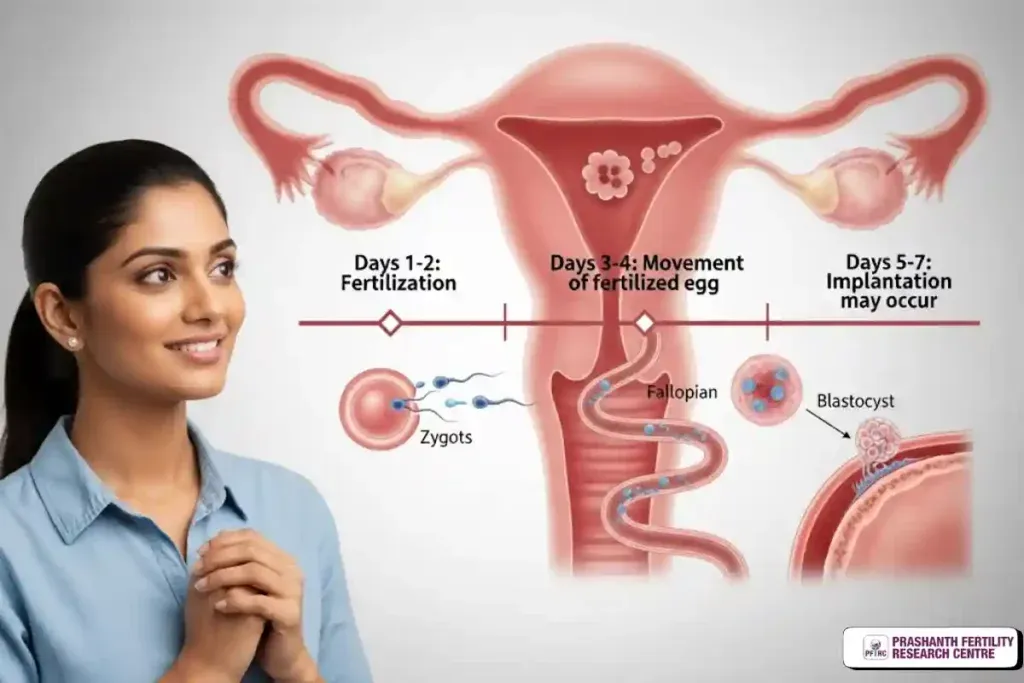
In-vitro fertilization, or IVF, is a more complex form of fertility treatment that involves retrieving eggs from a woman’s ovaries and fertilizing them with sperm in a laboratory. This process is used when other fertility treatments have not been successful or when there are underlying medical conditions that make it difficult for a woman to conceive naturally.
The first step in IVF is ovarian stimulation, where a woman takes medication to encourage her ovaries to produce multiple eggs. Once the eggs reach maturity, they are retrieved through a minor surgical procedure. The eggs are then fertilized with sperm in a laboratory, and the resulting embryos are monitored for a few days. The healthiest embryos are then transferred into the woman’s uterus, where they can hopefully implant and result in a pregnancy.
The Outcomes of Artificial Insemination and IVF
The success rates of artificial insemination and IVF vary depending on various factors such as the age and health of the woman, the quality of the sperm and eggs, and the specific fertility clinic. Generally, the success rates for artificial insemination are lower than those of IVF, with IUI having a 10-20% success rate and IVF having a 40-60% success rate.
However, both methods have helped countless couples and individuals achieve their dreams of starting a family. Many couples who have undergone artificial insemination or IVF have been able to conceive and give birth to healthy babies. These procedures have also allowed same-sex couples and single individuals to become parents, breaking down traditional societal norms of what a family should look like.
Bringing Home a Baby: The Outcome of Artificial Insemination and IVF
The emotional impact of these procedures cannot be overlooked. For couples who have been struggling with infertility, artificial insemination and IVF offer a glimmer of hope and a chance for them to fulfill their desire to have a child. While the process can be physically and emotionally taxing, the end result of holding their baby in their arms makes it all worth it.
Challenges and Considerations
While artificial insemination and IVF have brought joy and happiness to many families, there are also challenges and considerations that come with these procedures. The cost of these treatments can be significant, with IVF being more expensive than artificial insemination due to the complexity of the process. Insurance coverage for fertility treatments also varies, making it inaccessible for some couples.
Another consideration is the potential for multiple births with IVF. Because multiple embryos are often transferred to increase the chances of success, there is a higher likelihood of twins, triplets, or more. While this may seem like a blessing, it can also bring about financial, emotional, and physical challenges for the parents and the babies.
Additionally, the success rates of these procedures decrease with age, making it more difficult for older couples to conceive through artificial insemination or IVF. It is essential for individuals and couples to discuss their options with a fertility specialist and understand the potential challenges and risks before embarking on these treatments.
The Impact on Families
The decision to undergo artificial insemination or IVF is a personal one and can have a profound impact on families. For couples struggling with infertility, these procedures offer a ray of hope and can bring them closer together as they navigate the process together. For same-sex couples and single individuals, it can provide an opportunity to fulfill their dreams of becoming parents and create a loving and supportive environment for their child.
However, there can also be challenges that come with these procedures, such as the financial strain and emotional toll it can take on a couple. It is crucial for families to have a support system in place, whether it be through family and friends or a support group, to help them through the ups and downs of the fertility journey.
In the end, the outcome of artificial insemination and IVF is a beautiful, healthy baby, and for many families, that is all that matters. These procedures have given hope and joy to countless couples and individuals and have allowed them to experience the miracle of bringing a child into the world.
In conclusion, artificial insemination and IVF have revolutionized the world of fertility treatments and have helped countless families achieve their dreams of having a child. While there are challenges and considerations that come with these procedures, the positive impact they have had on families cannot be denied. Whether it is through artificial insemination or IVF, the outcome of bringing a baby home is a joyful and life-changing experience that brings love, happiness, and fulfillment to all involved.
Summary: In this blog post, we explored the outcomes of artificial insemination and IVF and the impact they have on families who have chosen to use them to bring a child into their lives. We discussed the procedures and success rates of both methods, as well as the challenges and considerations that come with them. Ultimately, the decision to undergo these treatments is a personal one, but for many families, it has resulted in the beautiful outcome of bringing a healthy baby home.