Blog Post: The Impact of Donor Selection: Intrauterine Insemination vs Donor Insemination
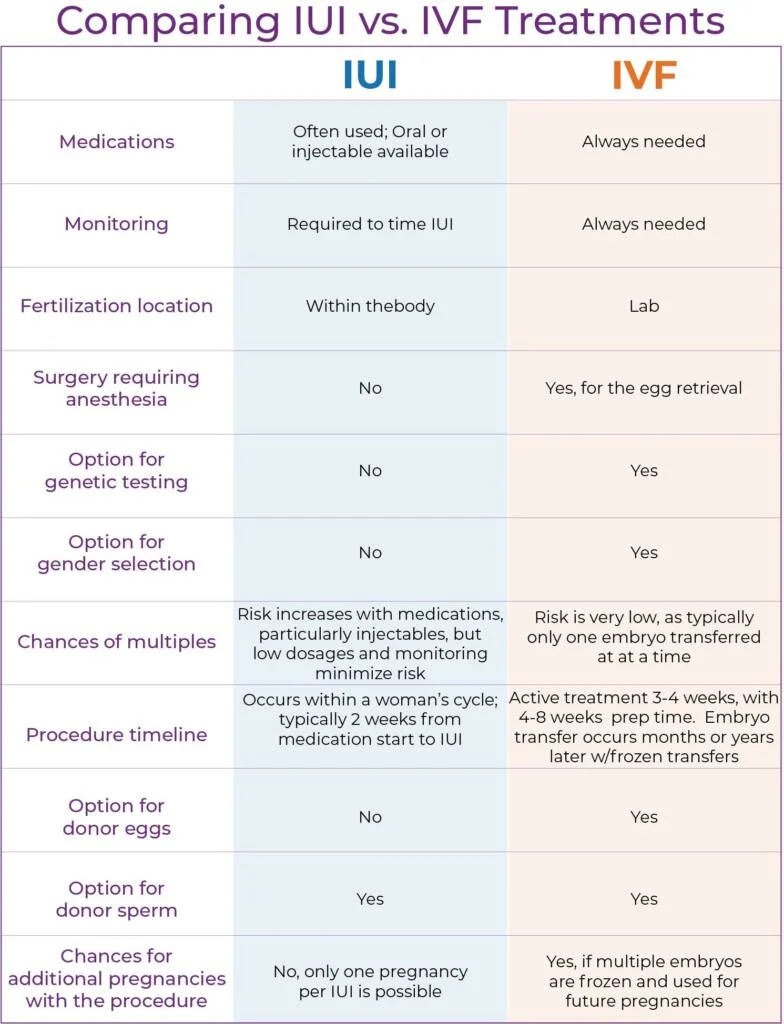
In recent years, there has been a significant increase in the use of assisted reproductive technologies to help couples conceive. One of the most commonly used methods is donor insemination, where sperm from a donor is used to fertilize the woman’s eggs. However, there is also a lesser-known technique called intrauterine insemination (IUI), which involves placing washed sperm directly into the uterus. Both of these methods have their own unique advantages and disadvantages, especially when it comes to donor selection. In this blog post, we will explore the impact of donor selection on the success rates and overall experience of both intrauterine insemination and donor insemination.
Intrauterine Insemination (IUI)
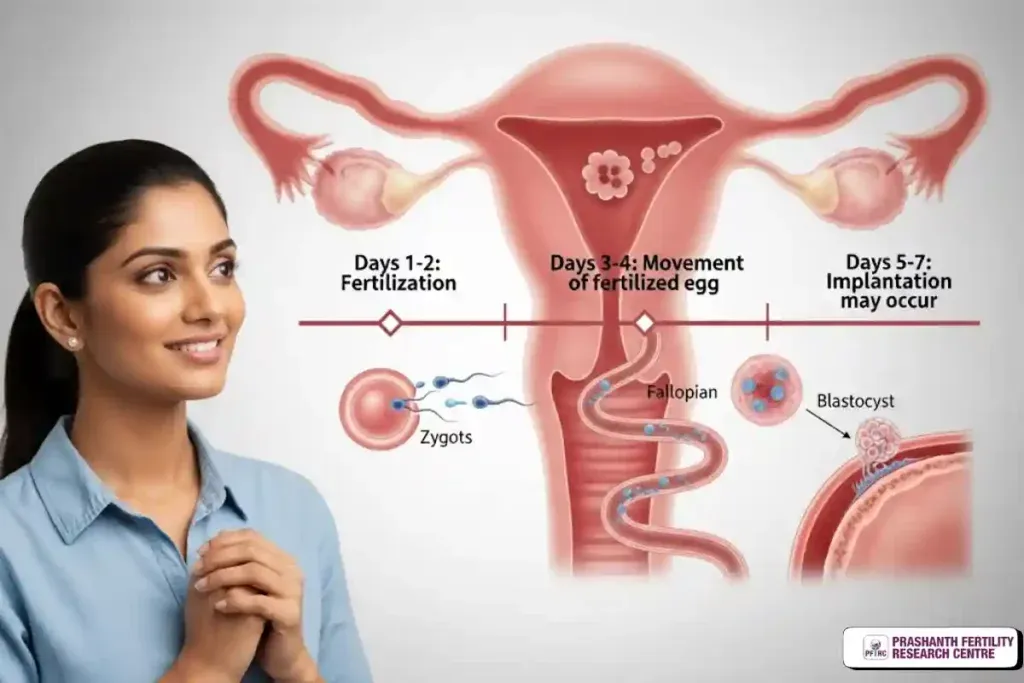
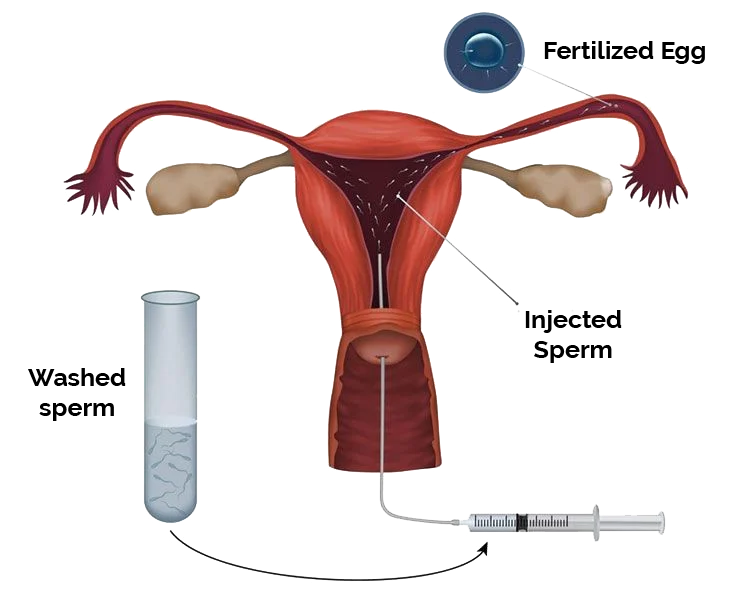
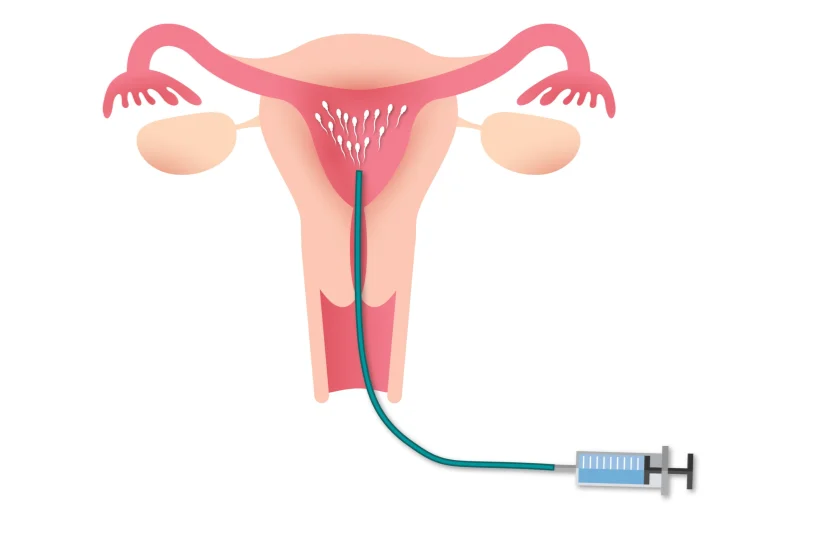
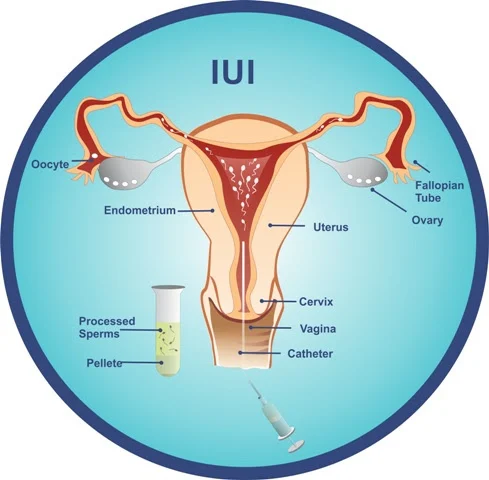
Intrauterine insemination, also known as artificial insemination, is a fertility treatment that involves placing washed sperm into the uterus through a thin catheter. This method is often used for couples who are experiencing male factor infertility or unexplained infertility. It can also be used for single women or same-sex female couples who require donor sperm to conceive.
When it comes to donor selection for IUI, the process is quite different compared to donor insemination. Unlike donor insemination, where the sperm donor is anonymous, IUI allows the couple to select a known donor, such as a friend or family member. This can be a significant advantage for the couple as they have the opportunity to choose someone they know and trust to be the biological father of their child.
However, this also means that the couple needs to carefully consider their choice of donor. Factors such as physical characteristics, medical history, and genetic screening all need to be taken into account. In addition, the donor must go through extensive testing to ensure that they are healthy and their sperm is of good quality. This can be a time-consuming and emotionally taxing process for both the couple and the potential donor.
Donor Insemination (DI)
Donor insemination, on the other hand, involves using sperm from an anonymous donor to fertilize the woman’s eggs. This method is often used for couples with severe male factor infertility, single women, or same-sex couples who require donor sperm to conceive. The sperm donor is carefully screened and selected by the fertility clinic, and the couple has no contact with the donor.
The Impact of Donor Selection: Intrauterine Insemination vs Donor Insemination
One of the major advantages of donor insemination is the anonymity of the donor. This can be beneficial for couples who do not want their child to have a known genetic connection to someone outside of their family. It also eliminates the need for the couple to go through the process of selecting and screening a known donor.
However, the lack of involvement in the donor selection process can also be a disadvantage for some couples. They may feel disconnected from the genetic makeup of their child, and the child may have questions about their biological father in the future. In addition, the limited information provided about the donor can be a concern for some couples, especially when it comes to potential genetic health risks.
Success Rates and Risks
When it comes to success rates, there is no significant difference between IUI and DI. Both methods have a similar success rate of around 20-25% per cycle. However, this can vary depending on factors such as the age of the woman, the quality of the sperm, and the reason for infertility.
One of the main risks associated with both IUI and DI is the potential transmission of genetic diseases. While donors are thoroughly screened, there is still a small chance that a genetic disease or disorder could be passed on to the child. This is why it is crucial for couples to carefully consider their donor selection and undergo thorough genetic testing.
The emotional impact of donor selection
The decision to use donor sperm for conception can be a challenging and emotional one for many couples. The process of selecting a donor, whether known or anonymous, can bring about feelings of uncertainty, anxiety, and even grief. It is essential for couples to discuss their feelings and concerns with each other and seek support from a therapist or support group if needed.
Furthermore, the child may also have questions and emotions surrounding their conception and the identity of their biological father. It is crucial for parents to be open and honest with their child about their origins and provide support and guidance as they navigate their feelings.
In summary, both intrauterine insemination and donor insemination are valid and effective methods of assisted reproduction. The choice between the two will ultimately depend on the individual needs and preferences of the couple. While IUI allows for a known donor and more involvement in the selection process, DI offers the advantage of anonymity. Regardless of which method is chosen, careful consideration and thorough screening of the donor is crucial for the health and well-being of the child.